
with the result in the correct data format as outlined in Humanas standard file layout.
#HUMANA CORRECTED CLAIM TIMELY FILING LIMIT 2021 HOW TO#
If you are not yet contracted and would like more information on how to be, please visit your state's page under the "Plan Documents" section of this page. adjudication of claims for Medicare Advantage members.

Instructions are included in the application. The following credentialing application can be used to send us facility and ancillary provider credentialing information once your group is contracted with us. Application has been re-attested within the past 120 daysįacility & Ancillary Provider Credentialing.Devoted Health is authorized to access the application.Attachment could be a copy of claim with original print date, or screen print from billing system. Health Plan prior to the timely filing limit of six months from the date of. For a non-network provider, the benefit plan would decide the timely filing limits. Claim has never been timely filing requirement. Facility Claims Submission - Quick Reference Guide. Timely filing is the time limit for filing claims, which is specified in the network contract, a state mandate or a benefit plan. Late claim submission submitted and is past the. The CAQH profile is complete and contains all required information (including current malpractice insurance) Note: Document Control Number assigned by provider must exactly match as submitted on claim.To avoid delays in the credentialing process, please ensure the following: We utilize CAQH applications to complete credentialing.
If claims are submitted after this time frame, they will most likely be denied due to timely filing and thus, not paid. The rule change being posted for public comment is updating a specific paragraph in policy that had not been previously updated with the correct timely filing limit.Practitioner credentialing is initiated once a contract is executed and the practitioner is loaded into our system. 1 year ago Updated The following table outlines each payers time limit to submit claims and corrected claims. The timely filing period includes the submission of original as well as any subsequent corrected or replacement claims. The limit remains at 6 months from the date of service to submit a timely claim, and then once a claim is submitted timely, the provider has 6 more months to resubmit the claim if necessary, see OAC 317:30-3-11.1. Please include AB1629 in box 80 of your corrected claim Note. CPT only 2006 American Medical Association (or such other date. Refer to the Provider eManual (section 10.12.3) for additional corrected claim tips. TRICARE is a registered trademark of the Department of Defense (DoD), DHA. These rule changes do not change the timely filing limits in the main section of policy that deals with timely filing, OAC 317:30-3-11. corrected claim canceling charges for the original claim, AND Submit a new claim with the correct member ID number or date of service 7. New Jersey - 90 or 180 days if submitted by a New Jersey participating health care provider for a New Jersey line of business member. One would think 6 months would be ample time but as of late I have become increasingly skeptical in SSA's ability to assist a non-tech savvy citizen, or if the citizen has to troubleshoot their online SSA account. To be considered timely, health care providers, other health care professionals and facilities are required to submit claims within the specified period from the date of service: Connecticut - 90 days. To request an appeal of a denied claim, you need to submit your request in writing, via Availity Essentials or mail, within 60 calendar days from the date of the denial.
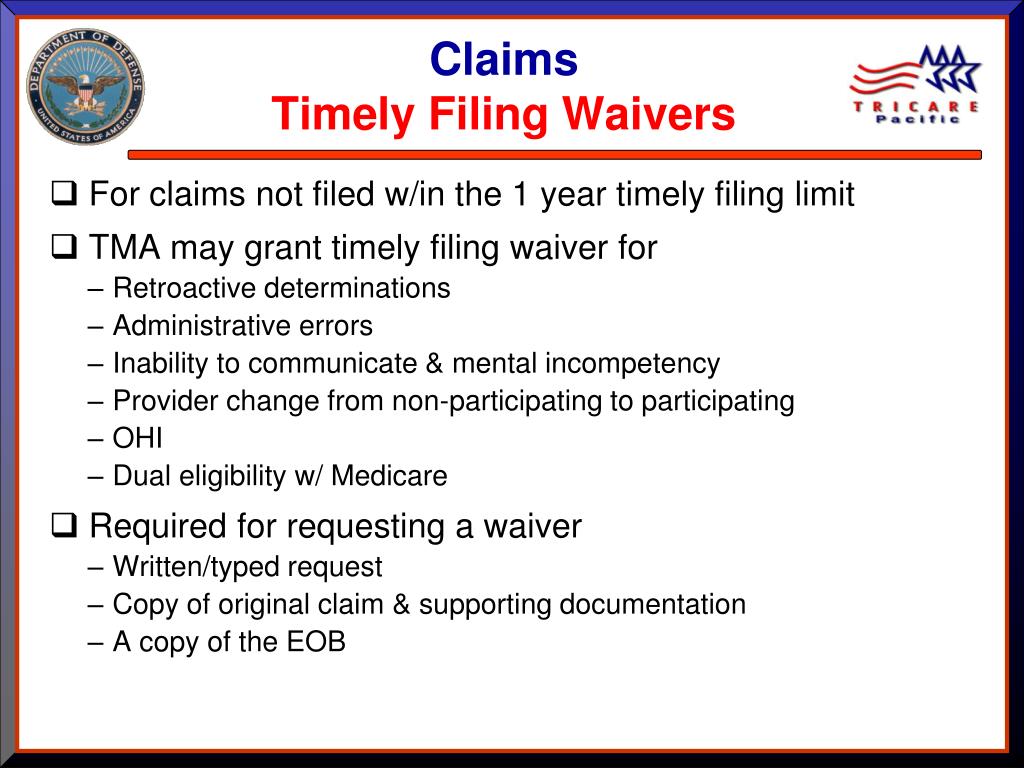
98 of claims must be paid within 30 days and 100 within 90 days. All claims must be submitted electronically in order to receive payment for services. TRICARE requires providers to file claims electronically with the appropriate HIPAA-compliant standard electronic claims format. If OKDHS is not able to verify someone's SSI through their means it can be a significant challenge on the client to acquire that information from the SSA to provide to OKDHS. Claims processing standards and HIPAA guidelines. Administratively, I think this makes sense, I am but slightly hesitant due to the challenges Social Security has had during the pandemic.


 0 kommentar(er)
0 kommentar(er)
