
Medical necessity determinations in connection with coverage decisions are made on a case-by-case basis. Please note also that the ABA Medical Necessity Guide may be updated and are, therefore, subject to change. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. The member's benefit plan determines coverage. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna) for a particular member. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. Members should discuss any matters related to their coverage or condition with their treating provider.Įach benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Treating providers are solely responsible for medical advice and treatment of members. The ABA Medical Necessity Guide does not constitute medical advice. The Applied Behavior Analysis (ABA) Medical Necessity Guide helps determine appropriate (medically necessary) levels and types of care for patients in need of evaluation and treatment for behavioral health conditions.
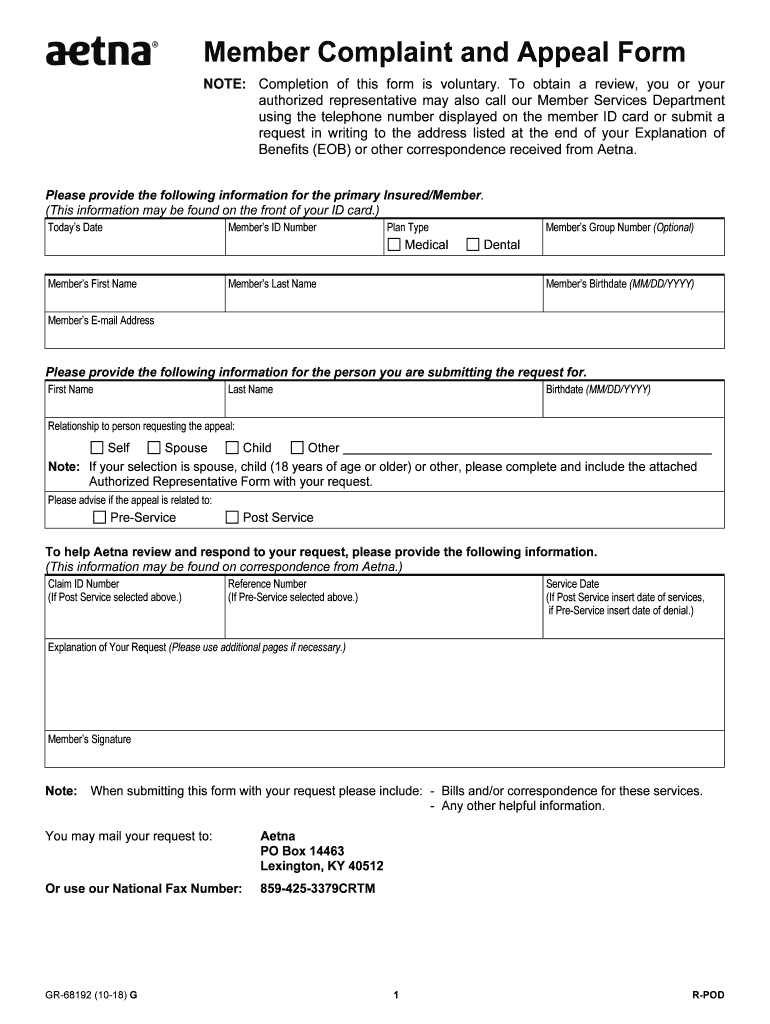

1-80$ for indemnity and PPO-based benefits plansīy clicking on “I Accept”, I acknowledge and accept that:.Or contact our Provider Service Center (staffed 8 a.m. Documents that support your position (for example, medical records and office notes).A copy of the denial letter or Explanation of Benefits letter.The reasons why you disagree with our decision.A completed copy of the appropriate form.To help us resolve the dispute, we'll need: Appeals: Requests to change a reconsideration decision, an initial utilization review decision, or an initial claim decision based on medical necessity or experimental/investigational coverage criteria.Reconsiderations: Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing.The timing of the review is prior to an appeal and incorporates state, federal, CMS and NCQA requirements. Peer to Peer Review - Aetna offers providers an opportunity to present additional information and discuss their cases with a peer-to-peer reviewer, as part of the utilization review coverage determination process.Health care providers can use the Aetna dispute and appeal process if they do not agree with a claim or utilization review decision.


 0 kommentar(er)
0 kommentar(er)
